Breathing more easily
Better preemie respiration monitoring through data analysis
The premature baby’s life is well monitored, but precarious.
Among the dangers that preemies face are episodes of central apnea. These periods in which the baby stops breathing can last 90 seconds or more. John Delos says that central apnea episodes are fairly common among preemies, but many of these episodes have gone unnoticed because when a baby has an apnea attack, it doesn’t always trip the respiration monitor alarm.
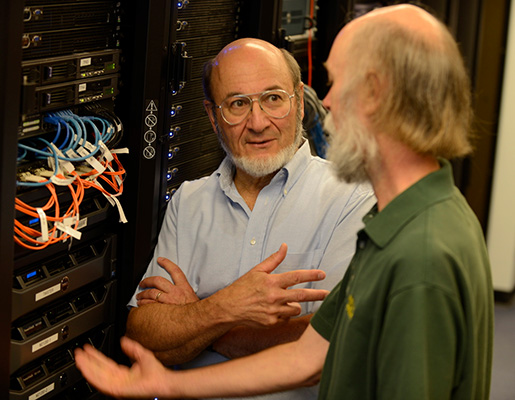
 Delos is a professor of physics at William & Mary. His research interests have centered on topics such as the physics of the hydrogen atom and chaotic transport, but he also employs his quantitative skills to analyze the data collected from monitors in neonatal intensive care units (NICUs).
Delos is a professor of physics at William & Mary. His research interests have centered on topics such as the physics of the hydrogen atom and chaotic transport, but he also employs his quantitative skills to analyze the data collected from monitors in neonatal intensive care units (NICUs).
Delos has been working on ways to use algorithms to improve NICU monitoring with a team that includes researchers from the University of Virginia and the UVA Health system. The project was supported by funding from the National Institute of Health’s National Institute of Child Health and Human Development.
Apnea paper wins prize
The collaborators had previously shown that monitoring the heart rates of newborns can give early warning of sepsis (bacterial infection). More recently, their paper in Physiological Measurement, “A new algorithm for detecting central apnea in neonates,” was awarded the 2013 Martin Black Prize for best paper of 2012 in the journal. Delos just returned from Brighton, UK, where he accepted the Martin Black Prize at the International Conference on Medical Physics on Sept. 3.
The new algorithm developed by the team, which included former William & Mary postdoc Hoshik Lee, is essentially a software filter that will allow the monitoring system to detect central apnea attacks more accurately by separating the signals for respiration and heartbeat.
Central apnea occurs in infants because the rhythm-generating system, which is located in the brain stem, is underdeveloped in preemies. By contrast the heart has a built-in pacemaker to set the pulse rate. Christopher Del Negro, in William & Mary’s Department of Applied Science, studies how the respiratory rhythm generation works.
The NICU monitor, fed by a set of three chest leads, is designed to do double duty, Delos explained. The EKG tracks the heart rate, and the monitor derives a respiration rate by measuring electrical resistance across the chest. ”Air is a poor conductor of electrical current, and when the baby inhales and exhales, the resistance rises and falls” Delos explained.
Circulation signal fools the monitor
The problem is that the monitor tracks the heart rate well, but is less reliable when it comes to respiration, and especially lack thereof. The researchers saw that during many central apnea attacks, the blood pumping through the heart fools the monitor into thinking that the baby is still breathing. Delos points to an EKG recording of a preemie.
“Here’s an example of a baby who, for no apparent reason, suddenly stops breathing,” Delos said. “The current generation of monitors, unfortunately, doesn’t recognize this. The heart beat also causes fluctuations in the electrical resistance, and the monitor confuses that with breathing. It says, no problem—this baby is now breathing at 175 breaths per minute. But babies can’t breath that fast.”
The NICU monitoring technology was developed in the 1970s to display a stream of vital signs in real time. “A clinician watching the monitor can see about a minute’s worth, or maybe at most five minutes’ worth. The information is displayed, but then it just gets thrown away, ” Delos explained. “This is an example of old technology that was the state of the art at its time. Today we can do much better.”
For one thing, it became practical to record—and analyze—all that information. Moore’s Law—the predicted doubling of computer memory capacity— caught up with the NICU monitors. Delos holds up a thumb drive: “This little thing? Sixteen gigabytes! A few hundred dollars gets you a terabyte,” he said. Delos said that Randall Moorman at the University of Virginia Health System, a co-author on the paper, was one of the first to realize the potential for collecting the firehose of NICU data.
“Randall had the vision to realize that there must be more information in those signals than people had been seeing, essentially because the signals were just going by,” Delos said. He explained that the EKG collects data at a rate of around 240 times each second.
“Storing 240 numbers per second is a big job after not all that many seconds. Now at last we can collect all that information, save it, and then go back and reanalyze it,” he said. “We have 240 numbers per second times three different pairs of leads, and that’s for about 40 infants for a period of about five years.”
Delos and his group acquired a large database: It amounted to five terabytes of clinical data in William & Mary’s SciClone Computing Complex. As they looked at the data, they knew that their challenge was to figure out a better way to distinguish breathing from heart rate—a knotty problem because pulse and respiration rates can put up similar numbers.
“The heart rate is constantly varying. It goes faster and slower. There is a broad frequency band representing the heart beat, and to filter it out is difficult,” he said. “Most importantly, if a baby stops breathing, the heart slows down. The rhythm can come right down into the breathing band.”
Borrowing an idea from Galileo
To parse respiration from heart rate, the researchers borrowed an idea from Galileo.
“He was sitting in church one day and there was a lantern swinging in the breeze,” Delos said. “Instead of paying attention to the Mass as he was supposed to, he started watching the swinging lantern.”
Galileo noticed that the lantern would swing a greater or lesser arc depending on the strength of the breeze—but the rhythm was the same. Delos said Galileo timed the lantern’s swings, using his own heartbeat as a clock.
“That was our idea, too: to use the heart as a clock,” he said. The monitors were giving all the necessary data already; Delos and his group used the EKG-generated rhythm as the basis of their new algorithm that allows for the separation of heart and respiration rates—and the reliable detection of central apnea events.
Delos said he and Lee accepted the award on behalf of the entire team that worked on the project.
“Part of the fun of this project has been working with a great variety of people with many different sets of skills, and all pulling together toward our goals,” he said.
In addition to Moorman, Delos noted that Doug Lake, the team’s statistician, was often the first to see the correlation between the electronic signals and the health of the patients. Postdocs Craig Rusin and Matt Clark set up the system for collection of the NICU signals as well as the clinical database.
“Terri Smoot, our research nurse, converted clinical information into electronic form, and Lauren Guin, undergraduate, helped with everything,” Delos said. “Brooke Vergales, Alix Paget-Brown and John Kattwinkel, neonatologists, explained to us what we were seeing—and its significance.”
More data, more information
Delos said that since the paper was published, he and his collaborators have used their algorithms and plumbed their large databases to get better information about the accuracy of nursing records, the effects of blood transfusions on apnea and how apnea changes according to the age of the patient.
“More important, we have developed new methods to study cardiorespiratory coupling and we have discovered an unexpected number of cases of extreme apnea—lasting more than 60 seconds,” he said. “Also, we are beginning a study of periodic apneas, which had long thought to be benign, but which in extreme cases, appear to provide early warning of pathological conditions.” ![]()